Get Healthy!
Staying informed is also a great way to stay healthy. Keep up-to-date with all the latest health news here.
04 Mar
Younger Adults Face Growing Threat From Colon and Rectal Cancer
A new report from the American Cancer Society finds colorectal cancer is increasingly affecting younger adults. The analysis also highlights rising rectal cancer cases, late diagnoses in people under 50, and ongoing gaps in screening.
03 Mar
New Global Analysis Warns of Sharp Rise in Breast Cancer Cases
The number of new breast cancer cases worldwide is predicted to surpass 3.5 million by 2050. But researchers say targeting six lifestyle risk factors could help change the trajectory.
02 Mar
Are Gut Microbiome Kits Overpromising?
The American Gut Project tests 21 at-home gut microbiome kits from seven companies and finds “major discrepancies.”
Rising Tree Pollen Counts Signal Start of Allergy Season
If you live in parts of the West and South, you may already be reaching for your allergy meds.
Tree pollen is ramping up in those regions, according to AccuWeather.com, which issued its 2026 pollen forecast on Wednesday.
"Temperature, rainfall, wind and springtime frosts all influence how much pollen ends up in the air," it sai...
- Carole Tanzer Miller HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Finding the Right Supportive Footwear for Pain Relief is Key, Say Podiatrists
If you suffer from persistent foot or lower body discomfort, the solution might be found in your closet rather than your medicine cabinet.
Podiatrists emphasize that the right footwear does more than just cushion your steps: It serves as a medical tool that can improve your overall physical health.
While many people associate o...
- Deanna Neff HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Fewer Mothers Died During Pregnancy or After Birth in 2024
Deaths linked to pregnancy and childbirth fell slightly in the United States in 2024, new data show. Early data suggests the decrease may have continued into 2025.
The U.S. Centers for Disease Control and Prevention (CDC) reported that 649 women died during pregnancy or within weeks after giving birth in 2024. That’s lower than the 6...
- HealthDay Staff HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Trader Joe’s Pulls Frozen Meals Tied to 37 Million-Pound Nationwide Recall
Trader Joe’s is recalling several frozen food items after reports that they may contain small pieces of glass.
The grocery chain said four frozen products could be affected and asked customers not to eat them.
The recall is linked to a much larger recall involving nearly 37 million pounds of food made by Ajinomoto Foods, ...
- HealthDay Staff HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
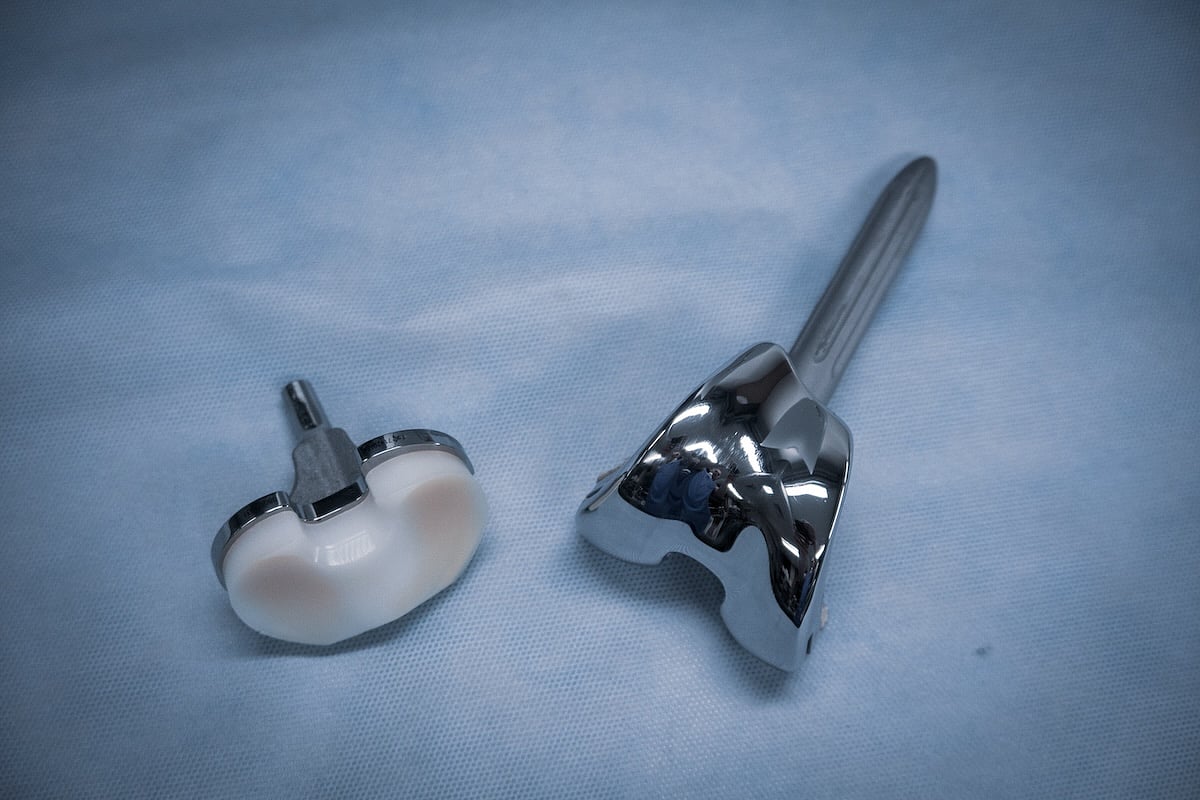
Testosterone Therapy Could Mean Trouble For Knee Replacement Patients, Study Warns
Testosterone therapy is booming in the U.S., but it might bring higher risks for people undergoing knee replacement surgery, a new study says.
Patients who took testosterone within a year of their surgery had a higher risk of infection, blood clots, kidney damage, pneumonia and knee instability after the procedure, researchers reported thi...
- Dennis Thompson HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Dentists Can Help Detect Undiagnosed Diabetes, Study Argues
Dentists might be able to help detect diabetes among their patients with a simple chairside test, a new study says.
A finger-prick blood test taken during dental exams found that more than 1 of 3 dental patients had elevated blood sugar levels consistent with either diabetes or prediabetes, researchers will report in the April issue of the...
- Dennis Thompson HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Ultra-Processed Foods Linked To Emotional, Behavioral Problems In Preschoolers
Ultra-processed foods can have an impact on a young child’s emotional and behavioral development, a new study says.
Kids who eat more ultra-processed foods have a higher risk of problems like anxiety, fearfulness, aggression or hyperactivity, researchers reported March 3 in JAMA Network Open.
In fact, for every 10% inc...
- Dennis Thompson HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Study Links Rising Cannabis Use to Poor Mental Health
For many, cannabis is a go-to for stress relief, but a large Canadian study suggests that for many, that fix may be closely tied to a worsening mental health crisis.
Researchers have found that as cannabis use becomes more common and weed more potent, the link between the drug and serious mood disorders is intensifying.
The study &md...
- Deanna Neff HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Fitness Trackers Might Help Predict Multiple Sclerosis Progression
Wrist-worn fitness tracking devices might be able to predict whether a person with multiple sclerosis is more likely to have worsening disability, a new study says.
Data from fitness trackers showed not only who was at higher risk of disease progression, but whose brains might be in danger of deterioration, researchers reported March 4 in ...
- Dennis Thompson HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Half of Americans Unaware of At-Home Colon Cancer Screening Options
Colon cancer is now the deadliest cancer for adults under 50, yet it remains one of the most preventable since polyps detected and removed during screening can’t turn into cancer later.
But a new nationwide survey commissioned by the Colorectal Cancer Alliance reveals a troubling reason why colon cancer death rates are on the rise: M...
- Deanna Neff HealthDay Reporter
- |
- March 5, 2026
- |
- Full Page
Review of U.S. Measles Elimination Status Delayed Until November
An expected review of the United States’ measles elimination status has been postponed by seven months.
The meeting, originally scheduled for mid-April, will now take place in November, according to the Pan American Health Organization (PAHO), a regional branch of the World Health Organization.
Measles has been considered elimi...
- HealthDay Staff HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
Your Furry Roommate May Be Affecting The Air You Breathe
Dogs may bring more than companionship into a home: They can also affect the air we breathe indoors, a new study shows.
Researchers found that dogs release airborne particles, gases and microbes that can affect indoor air quality. In some cases, the levels were similar to, and sometimes higher than, what humans release.
The findings ...
- HealthDay Staff HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
About 81,000 Baby Monitors Recalled Over Possible Fire Risk
Parents who use baby monitors may want to take a closer look at the one they have at home.
The U.S. Consumer Product Safety Commission (CPSC) has announced a recall of about 81,000 babysense Max View Baby Monitors because the display unit can overheat and create a possible fire hazard.
The monitors are made by Hisense, which has rece...
- HealthDay Staff HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
Two Days of Oatmeal May Lower Cholesterol, Study Finds
Whether topped with fruit or flavored with peanut butter, eating mostly oatmeal for just two days may help lower cholesterol, according to a new study out of Germany.
In the trial, people with metabolic syndrome who followed a strict oat-based plan for 48 hours saw a 10% drop in harmful LDL cholesterol.
The improvement was still noti...
- HealthDay Staff HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
Early Sports Specialization Linked To Increased Injury Risk
Parents of athletic children can protect them from injury by encouraging them to try out a wide variety of sports, a new study says.
Repetitive stress from focusing on one sport at a young age increases an athlete’s risk of injuries into adulthood, according to a pair of new studies presented this week at the American Academy of Orth...
- Dennis Thompson HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
More Kids, Teens Injured In E-Bike Wrecks, Study Finds
Electronic bikes, also referred to as e-bikes, are zooming in popularity, but they’re also responsible for more kids landing in an ER with injuries, a new study says.
E-bike injuries have more than tripled in San Diego in recent years, researchers reported Monday at a meeting of the American Academy of Orthopaedic Surgeons (AAOS) in ...
- Dennis Thompson HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
Exercise Boosts Quality of Life During Breast Cancer Chemotherapy
Extreme fatigue, muscle loss and psychological stress are well-known side effects of the chemotherapy that saves the lives of breast-cancer patients.
But should patients exercise during active phases of their treatment?
A new study provides additional evidence that movement may be one of the best ways to combat these challenges...
- Deanna Neff HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
Colorectal Cancer Rates Shifting to Younger Groups as Rectal Cancer Rates Spike
Colon cancer, long considered a disease of the elderly, is increasingly striking younger Americans, according to a startling new report.
Nearly half of new colon cancer diagnoses — about 45% — now occur in people under 65, according to the report from the American Cancer Society (ACS).
This is a massive jump from 1995, wh...
- Deanna Neff HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
Lithium Might Slow Brain Decline Among Seniors, Pilot Study Shows
The mood disorder drug lithium might have brain benefits beyond simply warding off depression and anxiety, a new study says.
A pilot clinical trial has found that low-dose lithium tablets might help slow verbal decline among seniors with mild cognitive impairment, researchers reported March 2 in JAMA Neurology.
Seniors takin...
- Dennis Thompson HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page
Brain Chemical Provides A 'Pep In Your Step,' Experiment Shows
Have you ever found a “spring in your step” when you’re walking toward something you enjoy – a favorite food, a good friend, an entertaining activity?
That’s a dopamine surge hitting your brain, a new study says.
Dopamine – a brain chemical associated with reward – appears to prompt people to...
- Dennis Thompson HealthDay Reporter
- |
- March 4, 2026
- |
- Full Page